Healthcare systems are facing a significant challenge: Millions of people suffer from chronic conditions that consume 70% of the National Health Service budget. These numbers show why healthcare systems need to become more efficient. Remote patient monitoring platforms offer a promising solution, and the market has already reached $16.6 billion in 2020.
Our team at Bask Health has seen remarkable results from remote patient monitoring that reshapes the scene of healthcare delivery. Research proves these platforms can reduce hospital readmissions by up to 72% and boost health metrics like blood pressure and glycated hemoglobin levels. Patient acceptance of telehealth services has jumped from 11% before the pandemic to 46%, which shows how people have embraced remote monitoring solutions.
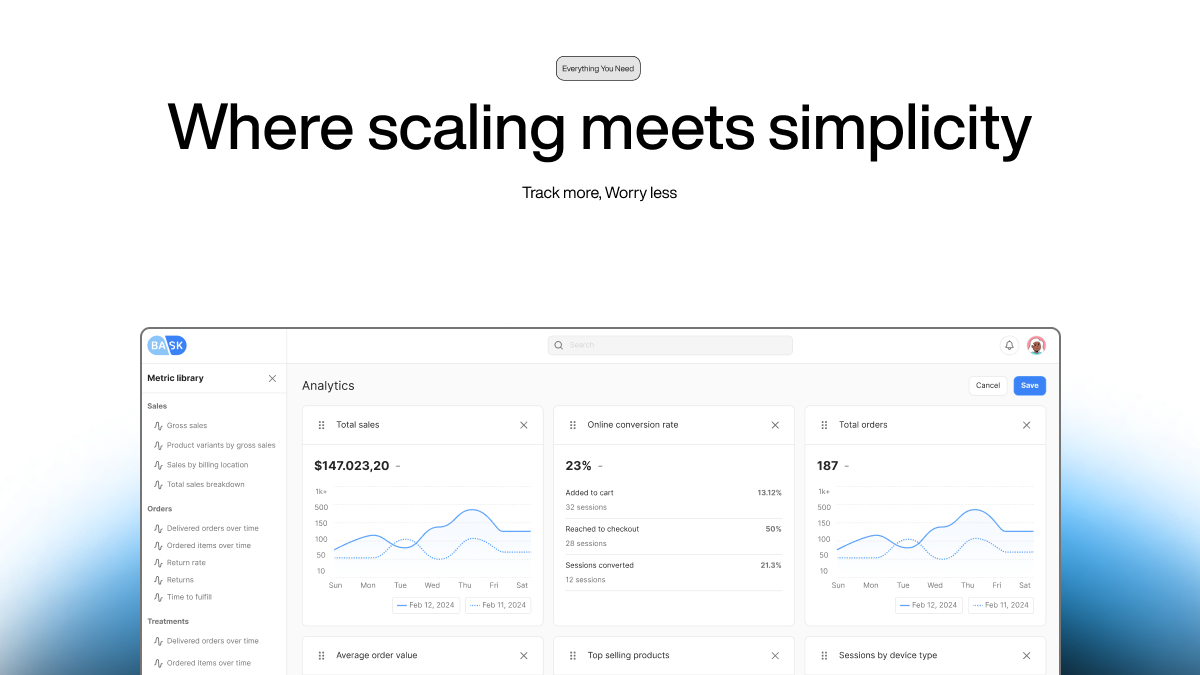
This piece will show you how our remote patient monitoring platform improves patient outcomes through up-to-the-minute data analysis, AI-powered analytics, and smooth EHR integration. You'll learn about implementing and scaling these solutions while you retain control of HIPAA compliance and measure success through specific metrics.
Key Takeaways
- Chronic Condition Management: RPM reduces hospital readmissions by up to 72% and improves vital health metrics.
- Patient Acceptance: Telehealth usage jumped from 11% to 46% post-pandemic, showing high patient acceptance.
- Real-Time Monitoring: Continuous data tracking via Bluetooth devices enhances patient care.
- AI-Driven Insights: Predictive analytics enable proactive health management.
- HIPAA Compliance: Advanced security measures ensure patient data protection.
- Seamless EHR Integration: Efficient data flow and alert systems improve clinical workflows.
- Staff Training: Comprehensive training boosts RPM adoption and effectiveness.
- Measuring Success: Metrics focus on patient engagement and improved clinical outcomes.
- Scalable Solutions: Strategic growth plans cater to diverse patient groups and device support.
Key Features of Modern RPM Platforms
Bask Health's remote patient monitoring platform has transformed healthcare delivery. Our platform usage jumped by 1,300% from 2019 to 2022. These numbers show how vital advanced monitoring has become in today's healthcare.
Real-time Patient Data Tracking Systems
Our platform tracks health data around the clock through Bluetooth-connected devices. Patients receive pre-configured tablets at home that collect vital health metrics and send them to our ClinicianConnect® portal. The system works with medical devices that track blood pressure, heart rate, blood oxygen levels, glucose levels, and other vital health markers.
Wireless-enabled sensors collect specific health data and store it in a relational database. Medical teams can look up single readings or review a patient's complete health history. The platform's two-way workflow connects smoothly with Electronic Medical Records (EMR) systems. This eliminates the need to enter data by hand.
AI-powered Health Analytics Tools
AI technology takes our monitoring capabilities to the next level. Smart algorithms scan huge amounts of patient data to spot tiny changes in vital signs. They often catch potential health issues before symptoms become obvious. The system builds personalized care plans based on each patient's medical history, vital signs, and lifestyle.
Our AI-powered predictive analytics can forecast health changes by looking at:
- Past patient records
- Current health measurements
- Environmental factors that matter
The AI systems have proven highly effective in helping doctors make decisions. They process vast amounts of clinical data that would take too long to review manually. Smart classification algorithms filter out data noise, which helps devices work better and monitor health more accurately.
HIPAA-compliant Security Measures
Patient data security sits at the heart of our platform design. We build protection into three key areas:
- Administrative Safeguards: Rules and steps that guide how we pick, develop, and update security measures
- Physical Safeguards: Protection systems that control physical access to electronic Protected Health Information (ePHI)
- Technical Safeguards: Digital tools that keep ePHI safe
Our encryption protocols shield patient information whether it's moving between systems or stored in databases. Strong access controls keep unauthorized users away from RPM devices and patient records, meeting strict HIPAA rules.
We run regular security checks to find weak spots and stay within HIPAA guidelines. The platform keeps detailed records of all security steps and watches compliance constantly to stay within HIPAA rules.
Business Associate Agreements (BAAs) extend our security framework to outside vendors. These agreements spell out exactly who handles PHI and how they must protect it. This complete approach makes sure everyone knows their role in protecting patient data and follows HIPAA rules carefully.
Setting Up Your Remote Monitoring System
Healthcare providers need careful planning and smart decisions to implement a successful remote patient monitoring system. Bask Health's experience has helped us identify the most important factors that will give a smooth integration of RPM platforms into existing healthcare workflows.
Platform Selection Criteria
The right RPM platform selection starts with assessing vendors on essential parameters. You should first assess how well the vendor can support your organization's implementation process. A detailed evaluation should be into:
- Integration capabilities with existing Electronic Health Record (EHR) systems
- Data security measures and HIPAA compliance protocols
- Technical support availability for staff and patients
- Device provisioning and maintenance services
Our research shows that 87% of patients can access smartphones and email. Platform compatibility with devices of all types is significant. Healthcare providers should offer both cellular and Bluetooth-enabled devices to match different patient priorities and technical capabilities.
Technical Requirements Assessment
Essential Technical Considerations:
- Data Transmission Infrastructure
- Check cellular network coverage in inpatient service areas
- Review Wi-Fi and Bluetooth connectivity requirements
- Set up secure data transmission protocols
- Device Management Systems
- FDA-cleared medical devices provide accurate monitoring
- Device provisioning and maintenance protocols
- Replacement and cleaning procedures
- Integration Requirements
- Single sign-on (SSO) capabilities
- Two-way data exchange mechanisms
- Custom API requirements
Real-world RPM implementation requires specific technical aspects. The Southmead rheumatology department's results stand out. They saved over 140 hours of clinic time and approximately $80,000 in unnecessary appointment costs through proper technical setup.
Our platform focuses on data governance compliance, especially when you have GDPR and HIPAA regulations. We create detailed flow diagrams of data movement and ensure appropriate security at each point. The platform maintains strict protocols for:
- Patient data storage and accessibility
- Regular security updates and patch management
- Ongoing service support and maintenance
Healthcare organizations can improve patient care delivery significantly through proper technical assessment and implementation. The Southmead case proves this success. They enrolled over 1,100 patients and completed more than 40,000 electronic Patient-Reported Outcome Measures (ePROMs) by mid-2023.
Integrating RPM with Existing Healthcare Systems
Healthcare systems need careful attention to detail for successful integration of remote patient monitoring platforms. Our experience at Bask Health shows that 96% of hospitals use certified EHR technology. This makes continuous connection vital to delivering optimal healthcare.
EHR Integration Steps
Our platform offers two main ways to integrate. The first option lets users view and change data among other clinical elements in the EHR system. The second provides data access through secure website links inside the EHR. We create direct communication channels between systems through open Application Programming Interfaces (APIs) and EHR marketplaces.
The integration process consists of:
Data Flow Configuration
Our platform's data flow setup gives smooth transmission of patient information. Full integration works in nine out of ten systems. This enables automated e-mails or EHR in-basket messages when values hit certain thresholds. The setup includes:
Automated Alert Systems: Clinical teams get notifications when symptoms cross predefined scores. These instant alerts lead to quick follow-ups by treating clinicians or nurses to intervene at the right time.
Consultation Workflows: Five systems use consultation-only workflows where clinicians check symptom data during clinic visits. This makes informed discussions and patient decision-making easier.
Staff Training Requirements
RPM implementation needs detailed staff training. We focus on four key areas:
- Technical Proficiency: Simple technology skills for new clinicians that include privacy, consent, and communication protocols.
- Advanced Communication: Experienced clinicians learn to maintain rapport and stay attentive in remote settings.
- Clinical Judgment: Training helps with complex decisions and coordination of multi-professional care in distributed settings.
- Implementation Skills: Staff learns to add remote visits into practice workflows and handle digital inequalities.
Practical training works better than just teaching theory. Team training, case discussions, and joint clinical sessions prove most effective. Trainees learn by watching experienced clinicians during consultations and then have one-on-one sessions.
Our training program includes regular feedback. Clinical trainers offer immediate "just ask" chances and group case discussions. This helps staff become skilled at using the system while maintaining efficiency.
Healthcare providers achieve remarkable results with proper integration and training. Studies show that well-integrated RPM systems help healthcare professionals detect and respond faster to patient needs. This improves care delivery and patient outcomes.
Measuring RPM Platform Success
Success in remote patient monitoring depends on patient engagement and clinical outcomes. Our work at Bask Health has helped us identify the most effective ways to measure RPM results.
Patient Engagement Metrics
Patient activation is vital to RPM success. Patients who actively participate show better adherence to treatment plans and get better health outcomes. We measure patient engagement in several ways:
Activation Levels: The Patient Activation Measure (PAM) evaluates patients' knowledge, skills, and confidence to manage their health. Higher activation levels are associated with better health outcomes and lower healthcare costs.
Portal Utilization: High portal adoption shows how much patients participate in their healthcare experience. Our data reveals that patients who check their health information through portals regularly show:
- Better medication adherence
- Better communication with healthcare providers
- A clear understanding of their treatment plans
Retention Metrics: Patient retention is a vital indicator of program success. We track patients at 30, 60, and 90 days, up to one year. This gives us a clear picture of long-term engagement patterns.
Clinical Outcome Improvements
Our platform has shown remarkable results in clinical parameters:
Blood Pressure Management: Patients with Stage 2 hypertension saw major improvements:
- Systolic blood pressure dropped by 23.8 mmHg
- Diastolic blood pressure fell by 14.5 mmHg
Mobility Outcomes: Studies of our RPM interventions revealed:
- Rehabilitation patients walked longer distances than non-monitored groups
- Better mobility shown in 6-minute walking tests
- Heart failure patients had better functional status
Chronic Disease Management: Our platform works well for many conditions:
- Type II diabetic patients reduced fasting blood glucose by 16.5 mg/dL
- Severe hyperglycemic patients lowered readings by 56.8 mg/dL
- 81.4% of weight management patients achieved lasting reductions
Our RPM platform's success depends on four key factors. Patients must use the technology as prescribed. Data transmission to providers needs to be continuous and secure. The system should detect abnormal readings quickly. Medical staff should respond fast through automated alerts and medication adjustments.
We measure success through numbers and quality assessments. Our continuous monitoring ensures the RPM platform delivers better patient care while keeping patients engaged.
Scaling Your Remote Monitoring Program
Remote patient monitoring adoption has surged dramatically, showing a sixfold increase from 2019 to 2022. This growth highlights why Bask Health must scale strategically. We plan to expand our services while ensuring quality care delivery as patient populations grow.
Adding New Patient Groups
We aim to expand by focusing on patients who get the most value from RPM services. Our data shows remote monitoring works best for:
Our analysis shows that 43% of patients need extra support to use all RPM features properly. This led us to create complete patient engagement protocols that help ensure steady technology use and smooth data flow.
Expanding Device Support
Our device ecosystem grows steadily as we add new FDA-approved monitoring tools. Our current device lineup has:
Core Monitoring Devices:
- Blood pressure cuffs
- Glucometers
- Pulse oximeters
- ECG + digital stethoscopes
- Wearable technology
- Digital thermometers
- Smart scales
We offer both cellular and Bluetooth-enabled options to make access easier. This two-pronged approach meets different patient priorities. Cost management remains vital since equipment prices have dropped to about $100 per device.
Resource Allocation Planning
Scaling successfully needs precise resource management. Our complete staffing model shows that RPM programs work best with 30-40 dedicated staff members who can handle 5,000-10,000 patients.
Critical Resource Components:
- Clinical Staff: Teams dedicated to patient monitoring and follow-up
- Technical Support: Round-the-clock help for device issues
- Quality Assurance: Teams that ensure program compliance and effectiveness
Medicare's expanded coverage rules helped us streamline our resource allocation. Policy experts still stress the need to "rightsize" service use - finding the sweet spot between access and cost.
Our platform uses generative AI tools to handle growing data streams. This technology helps clinical teams process huge amounts of patient data efficiently, which supports sustainable growth.
Mutually beneficial alliances with external monitoring services have boosted our ability to adjust medications based on remote data. This teamwork approach particularly helps blood pressure monitoring programs, where virtual teams collaborate with primary care providers to improve patient outcomes.
Conclusion
RPM platforms have shown their value by improving healthcare delivery and patient outcomes. Bask Health's experience shows how these solutions cut hospital readmissions and boost vital health metrics in patients of all types.
Research confirms our complete approach works. Blood pressure management improved with reductions of 23.8 mmHg in systolic pressure. We've also made great strides in chronic disease management. These results come from our platform's strengths: immediate data tracking, AI-powered analytics, and secure HIPAA-compliant infrastructure.
Here's what makes our platform work:
- The right platform that matches organizational needs
- Smooth EHR integration with standard protocols
- Well-designed staff training programs
- Smart growth strategies that stay eco-friendly
RPM technology will shape the future of healthcare delivery. Bask Health stands by its steadfast dedication to equipping healthcare providers with advanced monitoring tools that keep patient data secure and participation high. We help healthcare organizations deliver better patient outcomes, cut costs, and streamline care delivery through innovative implementation.
References
- American Medical Association (AMA). Remote patient monitoring implementation playbook overview. AMA Digital Practice Management. https://www.ama-assn.org/practice-management/digital/remote-patient-monitoring-implementation-playbook-overview. Accessed February 13, 2025.
- American Medical Association (AMA). Remote patient monitoring implementation playbook overview. AMA Digital Practice Management. https://www.ama-assn.org/practice-management/digital/remote-patient-monitoring-implementation-playbook-overview. Accessed February 13, 2025.
- Paubox. How to ensure HIPAA compliance when using RPM devices. Paubox Blog. https://www.paubox.com/blog/how-to-ensure-hipaa-compliance-when-using-rpm-devices. Accessed February 13, 2025.
- Tenovi. Remote patient monitoring program: Enhancing healthcare outcomes. Tenovi Blog. https://www.tenovi.com/remote-patient-monitoring-program/. Accessed February 13, 2025.
- PubMed Central (PMC). AI-driven remote patient monitoring: A systematic review. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC10711870/. Accessed February 13, 2025.
- PubMed Central (PMC). The effectiveness of remote patient monitoring in chronic disease management. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC7671621/. Accessed February 13, 2025.
- U.S. Department of Health and Human Services (HHS), Office of Inspector General (OIG). Additional oversight of remote patient monitoring in Medicare is needed. OIG Report. https://oig.hhs.gov/reports/all/2024/additional-oversight-of-remote-patient-monitoring-in-medicare-is-needed/. Accessed February 13, 2025.
- Bipartisan Policy Center. Maximizing the value of remote patient monitoring: Policy considerations and benefits. Bipartisan Policy Center Explainer. https://bipartisanpolicy.org/explainer/maximizing-the-value-of-remote-patient-monitoring/. Accessed February 13, 2025.
- American Medical Association (AMA). Remote patient monitoring implementation playbook overview. AMA Digital Practice Management. https://www.ama-assn.org/practice-management/digital/remote-patient-monitoring-implementation-playbook-overview. Accessed February 13, 2025.


